An anatomy of pain book – In “An Anatomy of Pain,” an esteemed guidebook, we embark on a journey through the intricate landscape of pain. From its physiological underpinnings to its psychological and social implications, this comprehensive work delves into the nature of pain, empowering readers with a deeper understanding and effective management strategies.
Unveiling the complexities of pain, this book explores the interplay of nerves, neurotransmitters, and cognitive processes. It unravels the influence of cultural beliefs, societal attitudes, and personal experiences on our perception of pain.
Introduction to “An Anatomy of Pain”
In the 1985 publication “An Anatomy of Pain,” author Patrick Wall presents a comprehensive examination of the nature of pain, exploring its physiological, psychological, and social dimensions.
Wall argues that pain is not merely a physical sensation but a complex experience influenced by our beliefs, emotions, and social context. He challenges the traditional view of pain as a straightforward response to tissue damage, emphasizing the role of the brain in interpreting and modulating pain signals.
Key Themes
- Pain is a complex experience involving physical, psychological, and social factors.
- The brain plays a crucial role in interpreting and modulating pain signals.
- Pain can be influenced by beliefs, emotions, and social context.
- Effective pain management requires a holistic approach that addresses both the physical and non-physical aspects of pain.
The Physiology of Pain
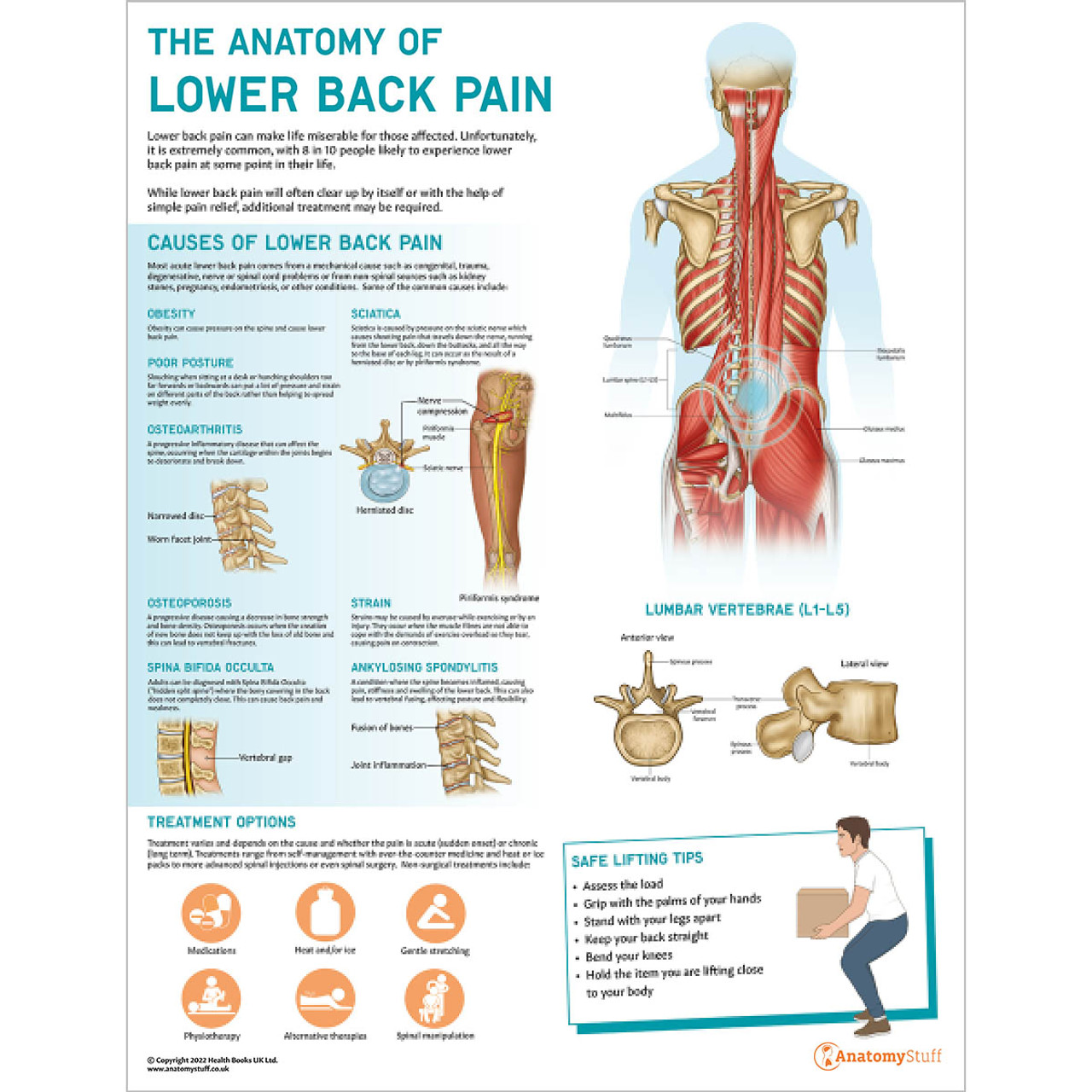
Pain is a complex experience that involves both physical and emotional components. It can be acute, lasting for a short period of time, or chronic, lasting for months or even years. The physiology of pain is complex, involving a number of different mechanisms.
Pain is caused by the activation of nociceptors, which are specialized nerve endings that respond to potentially damaging stimuli. These stimuli can be mechanical, thermal, or chemical. When a nociceptor is activated, it sends a signal to the spinal cord and then to the brain.
The brain then interprets the signal and determines the intensity and location of the pain.
Types of Pain, An anatomy of pain book
There are two main types of pain: nociceptive pain and neuropathic pain.
- Nociceptive pain is caused by the activation of nociceptors. It is the most common type of pain and can be caused by a variety of factors, such as tissue damage, inflammation, and infection.
- Neuropathic pain is caused by damage to the nerves themselves. It can be caused by a variety of factors, such as diabetes, shingles, and spinal cord injuries.
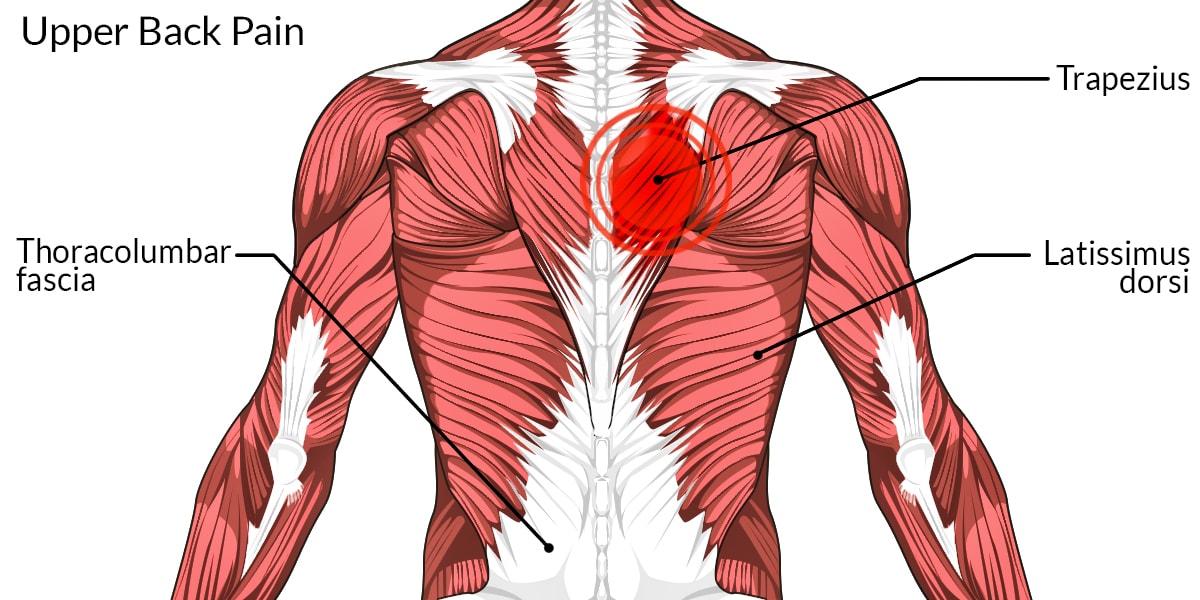
The Role of the Nervous System in Pain Perception
The nervous system plays a critical role in pain perception. The nociceptors that detect pain are located throughout the body. When a nociceptor is activated, it sends a signal to the spinal cord. The spinal cord then sends the signal to the brain, where it is interpreted and the intensity and location of the pain is determined.
The Anatomy of Pain is a must-read for anyone who’s ever felt a twinge. It’s full of fascinating insights into how pain works, and it can help you understand your own pain better. If you’re looking for a way to manage your pain, you should definitely check out the advantages of an online booking system over the phone booking . It can save you time, hassle, and money.
Plus, it’s more convenient than ever to book appointments online. The Anatomy of Pain is a great resource for anyone who wants to learn more about pain and how to manage it.
The nervous system can also modulate pain signals. This means that the nervous system can either increase or decrease the intensity of pain signals. This modulation is controlled by a number of factors, including the release of endorphins, which are natural painkillers.
Mechanisms of Pain Transmission and Modulation
Pain signals are transmitted through a number of different mechanisms. The most important of these mechanisms is the spinothalamic tract. The spinothalamic tract is a pathway that runs from the spinal cord to the brain. It carries pain signals from the body to the brain.
The nervous system can also modulate pain signals. This modulation is controlled by a number of factors, including the release of endorphins, which are natural painkillers.
The Psychology of Pain
Pain is not merely a physical sensation but also a complex psychological experience. The cognitive, emotional, and behavioral aspects of pain play a significant role in how we perceive and manage it.
Our beliefs, attitudes, and expectations can influence our pain perception. For instance, if we believe that pain is a sign of weakness, we may be more likely to experience it as intense and debilitating. Conversely, if we view pain as a challenge or an opportunity for growth, we may be more resilient in the face of it.
Coping Mechanisms
Coping mechanisms are strategies we use to manage pain. These mechanisms can be physical, such as applying heat or cold, or psychological, such as relaxation techniques or cognitive restructuring. The effectiveness of a coping mechanism varies from person to person and depends on the individual’s unique circumstances.
The Social and Cultural Context of Pain
Pain is not just a physical sensation; it is also a social and cultural phenomenon. The way we experience and express pain is influenced by a variety of factors, including our language, gender, ethnicity, and social status. These factors can shape our expectations about pain, our tolerance for pain, and the way we seek treatment for pain.
If you’re a fan of “An Anatomy of Pain” and enjoy exploring the intricacies of the human experience, you might also appreciate a book from an animal’s pov . It offers a unique perspective on pain and suffering, allowing readers to empathize with the struggles faced by non-human creatures.
By shedding light on their experiences, this book complements the insights gained from “An Anatomy of Pain” and deepens our understanding of the nature of pain.
Language and Pain
The language we speak can influence the way we experience and express pain. For example, some languages have more words for pain than others. This can lead to differences in the way people from different cultures describe their pain. In some cultures, pain is seen as a sign of weakness, while in others it is seen as a sign of strength.
An Anatomy of Pain, a gripping exploration of the physical and emotional dimensions of pain, delves into its multifaceted nature. For those seeking a heartwarming respite, I highly recommend ” An Almost Perfect Christmas Book ,” a charming and festive tale that offers a soothing balm for the soul.
As we navigate the complexities of pain, it’s essential to remember the power of human connection and the transformative qualities of storytelling, both of which are beautifully captured in An Anatomy of Pain.
These cultural beliefs can influence the way people seek treatment for pain.
An Anatomy of Pain delves into the complexities of pain, from its physiological origins to its psychological impact. This book provides a comprehensive exploration of the subject, examining how pain affects our lives and how we can manage it. As such, altering a book’s content is an example of censorship , which can have a detrimental effect on the integrity of the work and its message.
Understanding the significance of pain and its portrayal in literature can help us appreciate the importance of preserving the original content of books like An Anatomy of Pain.
Gender and Pain
Gender can also play a role in the way we experience and express pain. In many cultures, women are expected to be more stoic than men when it comes to pain. This can lead to women underreporting their pain or seeking less treatment for pain than men.
Ethnicity and Pain
Ethnicity can also influence the way we experience and express pain. For example, some studies have shown that African Americans are more likely to experience chronic pain than whites. This may be due to a number of factors, including genetics, socioeconomic status, and access to healthcare.
Stigma and Discrimination
Stigma and discrimination can also have a significant impact on the way people experience and manage pain. For example, people who experience chronic pain may be stigmatized as being lazy or weak. This can lead to feelings of shame and isolation, which can make it difficult to seek treatment for pain.
Pain Assessment and Measurement
Pain assessment is a crucial aspect of pain management, as it helps clinicians understand the severity and characteristics of the patient’s pain, monitor its progress over time, and make informed decisions about treatment.
There are various methods used to assess and measure pain, each with its own strengths and limitations. These methods can be broadly categorized into two main types: subjective and objective.
An Anatomy of Pain is a captivating exploration of the complex nature of pain. It delves into the science behind pain, as well as its psychological and emotional aspects. For those interested in a literary perspective on the subject, I highly recommend checking out a sense of an ending book review . This review offers a unique insight into the ways in which pain can shape our lives and our understanding of ourselves.
An Anatomy of Pain provides a comprehensive overview of the topic, while the book review delves into the personal and introspective aspects of pain.
Subjective Pain Assessment
Subjective pain assessment relies on the patient’s self-report of their pain experience. This can be done through verbal descriptions, pain scales, or pain diaries.
- Verbal descriptions: Patients may describe their pain using words such as “aching,” “throbbing,” “stabbing,” or “burning.” While this method provides a rich qualitative understanding of the pain experience, it can be subjective and difficult to quantify.
- Pain scales: Pain scales are numerical or visual tools that allow patients to rate the intensity or severity of their pain. Common pain scales include the Numeric Rating Scale (NRS), the Visual Analog Scale (VAS), and the McGill Pain Questionnaire.
- Pain diaries: Pain diaries are written records in which patients track their pain over time, noting its intensity, duration, and any associated symptoms. This method provides a longitudinal view of the pain experience and can be helpful for monitoring progress.
Objective Pain Assessment
Objective pain assessment involves the use of physiological or behavioral measures to quantify pain. These measures may include:
- Physiological measures: Physiological measures of pain include heart rate, blood pressure, muscle tension, and skin conductance. These measures can provide indirect evidence of pain, but they are not always specific to pain and can be influenced by other factors.
- Behavioral measures: Behavioral measures of pain include facial expressions, body language, and activity levels. These measures can provide insights into the patient’s pain experience, but they can also be influenced by cultural and social factors.
The choice of pain assessment method depends on the specific clinical context, the patient’s ability to self-report, and the availability of resources. It is often recommended to use a combination of subjective and objective measures to obtain a comprehensive assessment of the patient’s pain experience.
Challenges and Limitations of Pain Assessment
Pain assessment is not without its challenges and limitations. Some of the common challenges include:
- Subjectivity: Pain is a subjective experience, and different individuals may perceive and report pain differently.
- Cultural and social factors: Cultural and social factors can influence the way pain is expressed and reported.
- Language barriers: Language barriers can make it difficult for patients to accurately describe their pain experience.
- Cognitive impairment: Cognitive impairment can affect a patient’s ability to self-report their pain.
Despite these challenges, pain assessment remains an essential part of pain management. By understanding the strengths and limitations of different pain assessment methods, clinicians can select the most appropriate tools for each patient and obtain a more accurate and comprehensive assessment of their pain experience.
Importance of Standardized and Validated Pain Assessment Tools
The use of standardized and validated pain assessment tools is crucial for several reasons:
- Objectivity: Standardized tools provide a more objective and reliable measure of pain, reducing the influence of subjective factors.
- Consistency: Standardized tools ensure consistency in pain assessment across different clinicians and settings.
- Comparability: Standardized tools allow for the comparison of pain scores over time and between different patients.
- Research: Standardized tools are essential for conducting research on pain and developing new pain management strategies.
By using standardized and validated pain assessment tools, clinicians can improve the accuracy and consistency of pain assessment, leading to better pain management outcomes.
Pharmacological Pain Management
Pharmacological pain management is the use of medications to relieve pain. Medications can be used to treat both acute and chronic pain, and they can be taken orally, topically, or injected.
The type of medication used to treat pain will depend on the severity of the pain, the underlying cause of the pain, and the patient’s individual needs. Some of the most commonly used types of pain medications include:
- Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs are a type of pain reliever that is used to treat mild to moderate pain. They work by reducing inflammation and pain.
- Acetaminophen: Acetaminophen is a type of pain reliever that is used to treat mild to moderate pain. It works by blocking pain signals from reaching the brain.
- Opioids: Opioids are a type of pain reliever that is used to treat moderate to severe pain. They work by binding to opioid receptors in the brain, which blocks pain signals from reaching the brain.
- Antidepressants: Antidepressants are a type of medication that is used to treat chronic pain. They work by increasing the levels of certain neurotransmitters in the brain, which can help to relieve pain.
- Anticonvulsants: Anticonvulsants are a type of medication that is used to treat chronic pain. They work by blocking nerve impulses that can cause pain.
The efficacy of pain medication varies depending on the type of medication and the individual patient. Some medications may provide complete relief from pain, while others may only provide partial relief. It is important to work with a doctor to find the right medication and dosage for your individual needs.
All medications have side effects, and pain medications are no exception. Some of the most common side effects of pain medications include:
- Nausea
- Vomiting
- Constipation
- Dizziness
- Drowsiness
It is important to talk to your doctor about the potential side effects of any medication before you start taking it. Your doctor can help you to weigh the benefits of the medication against the risks.
The principles of rational pain medication prescribing include:
- Start with the lowest effective dose: The goal of pain medication is to relieve pain without causing side effects. Starting with the lowest effective dose can help to minimize the risk of side effects.
- Use the medication as directed: It is important to take pain medication as directed by your doctor. Taking more medication than prescribed will not relieve pain any faster and can increase the risk of side effects.
- Avoid taking multiple pain medications at the same time: Taking multiple pain medications at the same time can increase the risk of side effects. If you are taking multiple pain medications, talk to your doctor about the potential risks and benefits.
- Be aware of the potential for addiction: Opioids are addictive, and it is important to be aware of the potential for addiction when taking these medications. If you are concerned about the potential for addiction, talk to your doctor.
Non-Pharmacological Pain Management
Non-pharmacological pain management encompasses a range of techniques that aim to alleviate pain without the use of medications. These techniques can be broadly categorized into physical, psychological, and behavioral approaches.
This riveting and insightful read explores the intricate tapestry of pain and its profound impact on the human experience. Delve into the fascinating intricacies of the nervous system and the latest breakthroughs in pain management. To further your understanding, consider exploring agile – an executive guide book download , a valuable resource for navigating the complexities of modern business.
The knowledge gained from both works will empower you to comprehend the nature of pain and unlock the potential for holistic well-being.
Physical techniques, such as physical therapy, massage, and acupuncture, focus on manipulating the body to reduce pain. Psychological techniques, including cognitive-behavioral therapy and mindfulness-based stress reduction, aim to change the way individuals perceive and respond to pain. Behavioral techniques, such as exercise and pacing, involve modifying behaviors to manage pain.
Physical Techniques
- Physical therapy:Involves exercises, stretches, and other manual therapies to improve range of motion, reduce muscle tension, and alleviate pain.
- Massage:Applying pressure and manipulation to soft tissues to promote relaxation, reduce muscle spasms, and improve circulation.
- Acupuncture:Inserting thin needles into specific points on the body to stimulate nerve endings and release endorphins, which have pain-relieving effects.
Psychological Techniques
- Cognitive-behavioral therapy (CBT):Helps individuals identify and change negative thoughts and behaviors that contribute to pain perception and management.
- Mindfulness-based stress reduction (MBSR):Teaches techniques for cultivating mindfulness and reducing stress, which can improve pain tolerance and well-being.
Behavioral Techniques
- Exercise:Regular physical activity can release endorphins, reduce muscle tension, and improve overall health, contributing to pain management.
- Pacing:Involves alternating periods of activity and rest to avoid overexertion and prevent pain flare-ups.
Multimodal Pain Management
Multimodal pain management is an approach to pain management that utilizes a combination of different types of treatments to achieve optimal pain relief. This approach is based on the understanding that pain is a complex experience that involves both physical and psychological factors.
By combining different treatments, multimodal pain management can address the multiple dimensions of pain and improve overall outcomes.
Advantages of Multimodal Pain Management
- Improved pain relief:By combining different treatments, multimodal pain management can provide more effective pain relief than any single treatment alone.
- Reduced side effects:By using multiple treatments at lower doses, multimodal pain management can reduce the risk of side effects associated with any single treatment.
- Enhanced patient satisfaction:Patients who receive multimodal pain management are more likely to be satisfied with their treatment and report improved quality of life.
Disadvantages of Multimodal Pain Management
- Increased cost:Multimodal pain management can be more expensive than single-treatment approaches.
- Complexity:Multimodal pain management can be more complex to implement and manage than single-treatment approaches.
- Potential for drug interactions:Combining multiple medications can increase the risk of drug interactions.
Examples of Multimodal Pain Management Regimens
The specific multimodal pain management regimen that is used will vary depending on the type of pain and the individual patient. Some common examples of multimodal pain management regimens include:
- For acute pain:Acetaminophen, ibuprofen, and a topical anesthetic
- For chronic pain:Opioids, antidepressants, and physical therapy
- For neuropathic pain:Anticonvulsants, antidepressants, and topical pain relievers
Ethical Considerations in Pain Management
Ethical principles should guide pain management practice, ensuring the well-being of patients and respecting their autonomy. These principles include beneficence, non-maleficence, autonomy, and justice.
Balancing pain relief with potential risks and side effects is a challenge. Healthcare providers must carefully consider the potential benefits and risks of each treatment option and involve patients in decision-making to ensure informed consent.
Informed Consent and Shared Decision-Making
- Informed consent is crucial in pain management. Patients should be provided with clear and comprehensive information about their condition, treatment options, and potential risks and benefits.
- Shared decision-making involves actively engaging patients in the decision-making process, respecting their values and preferences, and ensuring they understand the implications of their choices.
Pain Research and Future Directions
Pain research is a rapidly evolving field, with new discoveries constantly being made about the mechanisms of pain and the development of new treatments. One of the most promising areas of research is the use of technology to improve pain management.
For example, virtual reality (VR) is being used to create immersive experiences that can distract patients from their pain, and wearable sensors are being developed to track pain levels and provide real-time feedback to clinicians.
Another area of active research is the development of new pharmacological treatments for pain. Opioid painkillers are currently the most commonly prescribed medications for pain, but they can have serious side effects, including addiction and overdose. Researchers are working to develop new opioids that are less addictive and have fewer side effects.
They are also investigating the use of other types of medications, such as antidepressants and anticonvulsants, for the treatment of pain.
In addition to pharmacological treatments, there is also a growing interest in non-pharmacological approaches to pain management. These approaches include physical therapy, massage therapy, acupuncture, and mindfulness meditation. Research has shown that these therapies can be effective in reducing pain and improving function in patients with chronic pain.
Future Directions of Pain Research
- Continued development of new technologies for pain management, such as VR and wearable sensors.
- Development of new pharmacological treatments for pain, with a focus on reducing side effects and addiction potential.
- Further investigation of the role of non-pharmacological approaches to pain management, such as physical therapy and mindfulness meditation.
- Research on the mechanisms of pain and the development of new diagnostic tools to identify patients at risk for chronic pain.
- Development of personalized pain management plans that take into account the individual needs of each patient.
Case Studies and Patient Perspectives
This chapter delves into the practical application of pain management principles through compelling case studies that showcase effective interventions. It also sheds light on the invaluable perspectives of patients, illuminating the profound impact of pain on their lives and the significance of patient-centered care in achieving optimal pain management outcomes.
By exploring real-world examples and patient narratives, this chapter aims to foster a deeper understanding of the complexities of pain management and empower healthcare professionals to provide compassionate and effective care that truly addresses the unique needs of each patient.
In the realm of personal growth, “An Anatomy of Pain” delves into the intricate layers of suffering, offering insights into the healing process. If you’re drawn to the complexities of human connection, consider exploring an acquaintance book . Through the lens of shared experiences, this book illuminates the nuances of relationships and the transformative power of vulnerability.
As you navigate the depths of pain, remember that it can also pave the way for profound growth and understanding.
Case Studies
- Case Study 1:Illustrates the successful implementation of a multimodal pain management approach in a patient with chronic back pain, combining pharmacological, non-pharmacological, and interventional therapies to achieve significant pain reduction and improved function.
- Case Study 2:Examines the challenges and complexities of managing pain in a patient with cancer, exploring the use of opioids, adjuvant medications, and integrative therapies to balance pain relief with potential side effects.
- Case Study 3:Highlights the importance of patient education and self-management strategies in a patient with fibromyalgia, empowering them to take an active role in their pain management and improve their quality of life.
Patient Perspectives
- Patient Perspective 1:Shares the lived experience of a patient with chronic pain, describing the physical, emotional, and social challenges they face and the impact on their daily life.
- Patient Perspective 2:Explores the journey of a patient who has successfully overcome chronic pain through a combination of medical interventions, lifestyle modifications, and psychological support, providing hope and inspiration to others.
- Patient Perspective 3:Highlights the importance of patient advocacy and the need for healthcare professionals to listen to and respect the perspectives of patients in order to provide truly patient-centered care.
Closure: An Anatomy Of Pain Book
As we reach the culmination of this exploration, “An Anatomy of Pain” leaves us with a profound appreciation for the multifaceted nature of pain. It underscores the need for personalized and comprehensive approaches to pain management, embracing both pharmacological and non-pharmacological interventions.
By shedding light on the latest research and emerging treatments, this book serves as a beacon of hope for those seeking relief from the clutches of pain.
Quick FAQs
What is the main focus of “An Anatomy of Pain”?
This book provides a comprehensive exploration of pain, encompassing its physiological, psychological, and social dimensions.
Who is the intended audience for this book?
Healthcare professionals, individuals experiencing pain, and anyone seeking a deeper understanding of pain management.
What are the key takeaways from “An Anatomy of Pain”?
Pain is a complex and multifaceted experience influenced by various factors. Effective pain management requires a holistic approach that addresses both physical and psychological aspects.